BEFAST: The critical upgrade transforming how strokes are recognized and treated

Spotting a stroke quickly can make all the difference between a full recovery and lifelong challenges. In the fast-paced world of emergency medical services, tools like BEFAST have stepped up to help paramedics and even bystanders identify these brain emergencies sooner and more accurately than older methods.
Decoding the BEFAST acronym
BEFAST breaks down into six straightforward checks anyone can do in under a minute. Each letter flags a classic stroke sign, starting with the newest additions that older tools missed.
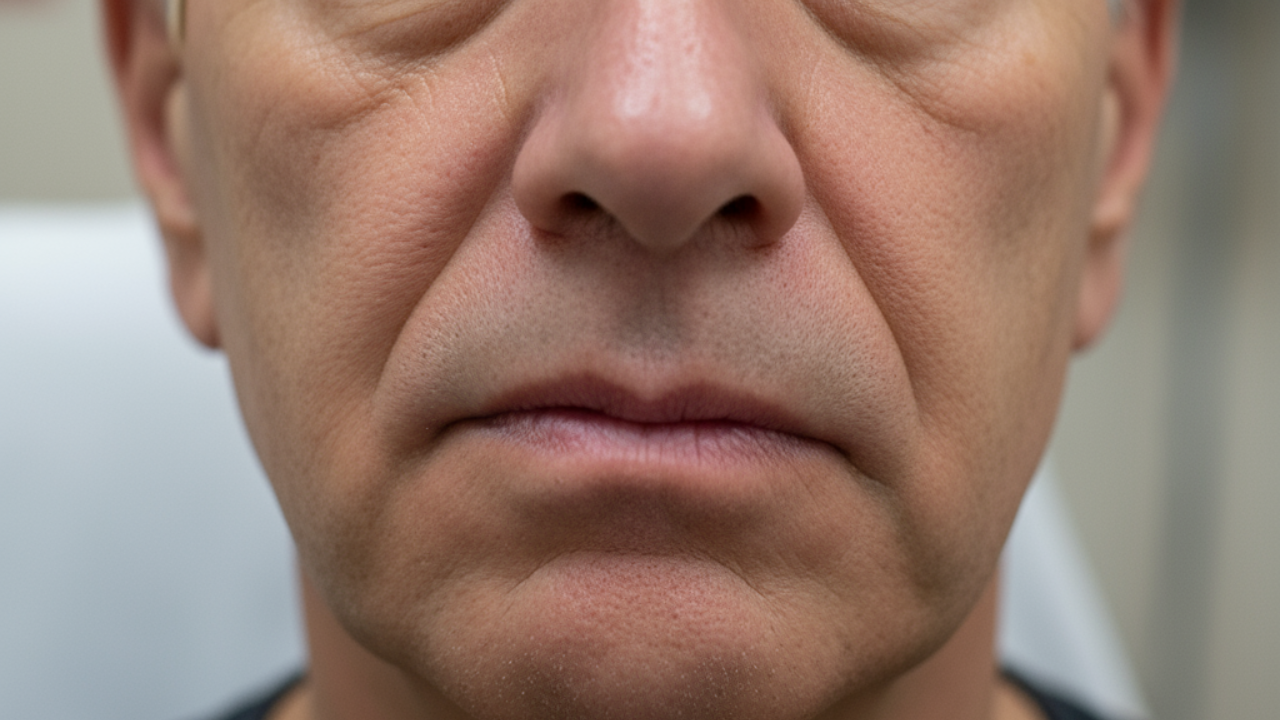
Balance comes first. Does the person suddenly seem unsteady on their feet, wobble when trying to walk straight, or struggle with coordination like touching their nose with their finger? These hint at strokes in the back of the brain, often mistaken for dizziness.Eyes follow. Look for sudden vision trouble, like double images, a lost patch in their sight, or blindness in one or both eyes. Blurry vision alone does not count as much; it is the sharp, new loss that screams stroke.Face droop shows when you ask them to smile or show their teeth. One side sags or stays flat while the other lifts normally.Arm weakness appears if they hold both arms out with palms up and eyes closed. One drifts down or they cannot keep it steady.Speech issues wrap up the core checks. Words slur, sentences garble, or they cannot grasp simple instructions or repeat a phrase like “The sky is blue.”Time seals it. Note the exact moment symptoms started or when they were last normal. Call emergency services right away, and share that timeline with responders.
How stroke care changed

Back in the early days of EMS, stroke calls were often treated as low priority. Care focused on support like oxygen and monitoring because no real treatments existed to reverse the damage. Things shifted dramatically in 1996 when alteplase, a clot-busting drug, got approved for acute ischemic strokes. Suddenly, speed became everything. Paramedics needed ways to spot strokes fast and rush patients to hospitals ready to act.The NIH Stroke Scale works great in hospitals but takes too long in an ambulance. So, simpler tools emerged. The Cincinnati Prehospital Stroke Scale checks for facial droop, arm drift, and speech issues. FAST made it even easier for the public: Face droop, Arm weakness, Speech trouble, and Time to call for help. These caught many strokes but missed others, especially those hitting balance or vision.
New treatments on the scene
Clot retrieval, or thrombectomy, changed the game again around 2015. Devices pull out large vessel blockages, effective up to 24 hours in select cases. But not every hospital does this. Primary stroke centers handle clot-busters; comprehensive ones add thrombectomy suites.Enter severity scales like RACE or LAMS. After a positive BEFAST, paramedics run these to score deficits. High scores suggest a large vessel occlusion needing a top-tier center. Dysarthria is slurred speech from motor issues; aphasia means trouble understanding or forming words, hinting at bigger cortical damage.Tenecteplase simplifies things further. Unlike alteplase’s hour-long drip, it is a single quick push, more targeted at clots, and less bleed-prone. Many protocols now favor it for its ease in the field.
Real-world impact

Picture a patient suddenly unsteady, seeing double, with a droopy smile and weak grip. BEFAST lights up positive. EMS alerts the hospital en route, grabs a severity score without delaying wheels-up, and heads to the right spot. Door-to-needle times drop, saving brain cells. About 1.9 million neurons die per untreated minute.Hemorrhagic strokes, around 13 percent of cases, bring thunderclap headaches or sky-high blood pressure. These go to neurosurgery-ready centers. Public awareness campaigns push BEFAST too, so families call early.EMS teams drill these tools relentlessly. Medical directors pick protocols, but the goal stays the same: thorough yet lightning-fast assessments. Half measures will not cut it when time truly is brain.Stroke care keeps advancing, but recognition starts with simple steps like BEFAST. Whether you are a paramedic racing lights-and-sirens or spotting signs at home, knowing it saves lives.